News and recovery-oriented commentary about current controversies, emerging trends and research findings related to drug and alcohol addiction, treatment and recovery.
Wednesday, October 29, 2008
Monday, October 27, 2008
McCain and Obama on drug policy
Addiction Inbox also has posts on both candidates.
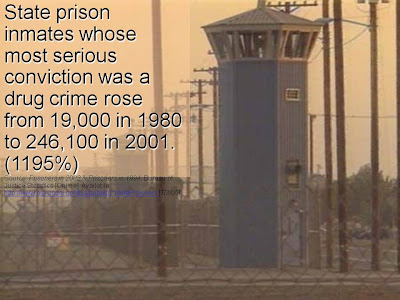
Bottom line: McCain wants to continue the drug war and Obama wants to promote drug courts and alternatives to incarceration.
Saturday, October 25, 2008
Things that make you go, "hmmm"
Aims: Attention-deficit/hyperactivity disorder (ADHD) is of great clinical importance not only because of its high prevalence but also due to the frequent comorbid illnesses that are connected with this disorder. Several studies were able to demonstrate that ADHD constitutes a significant risk factor for the exacerbation of habit-forming illnesses, i.e. addictions. Methods: We conducted a study on 152 adult patients with alcohol dependence (n = 91) or multiple substance addiction (n = 61) to determine whether or not these patients were affected by ADHD. For retrospective assessment of childhood ADHD, the WURS-k was used as well as the DSM-IV symptom checklist for ADHD. The CAARS was used to assess the persisting symptoms of ADHD in adults. Results: 20.9% (WURS-k) or 23.1% (DSM-IV diagnostic criteria) of the alcohol-dependent patients showed evidence of retrospective ADHD affliction in childhood. With the help of CAARS, ADHD was proved to be persistent in 33.3% of the adult patients. In the group of substance-addicted patients 50.8% (WURS-k) and 54.1% (DSM-IV) presented with diagnostic criteria for ADHD in childhood and 65.5% (CAARS) showed evidence of ADHD persisting in adulthood. Conclusions: These results reveal that habit-forming illnesses can be associated with a high comorbidity with ADHD, expressed in the form of alcohol abuse and also in consumption of illegal drugs. The results underline the great importance of early and adequate diagnostics and therapy of ADHD for the prevention of habit-forming illnesses.What I find remarkable is not the co-occurrence of ADHD and AOD problems. Rather, that this finding is accepted, and a finding of high intelligence among people with alcohol problems is met with such skepticism. What does this say about the researchers? What questions are they not asking, or at least taking seriously? Is this a case of the ladder of inference at work?
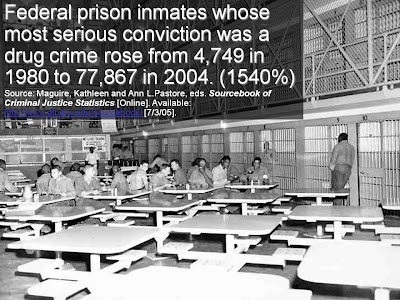
Narcotic Farm
About the lower image:From 1935 to 1975, just about everyone busted for drugs in the U.S. was sent to the United States Narcotic Farm outside Lexington, Ky. Equal parts federal prison, treatment center, research laboratory and farm, this controversial institution was designed not only to rehabilitate addicts, but to discover a cure for drug addiction.
...the institution became a premier center for research into drug addiction and treatment, advancingeverything from the use of methadone to treat heroin withdrawal to drugs that blocked the action of opiates. Along the way, Narco was frequented by legendary jazz musicians such as Chet Baker and Sonny Rollins, as well as actor Peter Lorre and beat generation writer William S. Burroughs, who recounted his experience in his first novel, Junkie.
The documentary also chronicles how the Farm was shut down when Congress discovered that researchers there were using patients as human guinea pigs in CIA-funded experiments into LSD. Drug research on federal prisoners is now illegal.
Still, the filmmakers note accomplishments at the institution remain milestones in addiction science and treatment. Its most important contribution might be how it transformed the way society views addicts—"as people suffering from a chronic, relapsing disorder that affects public health," says book co-author Nancy Campbell, an associate professor at Rensselaer Polytechnic Institute in Troy, N.Y., who studies the history of drug addiction research.
The original caption for this photo, which appeared in a 1951 New York World-Telegram & Sun series on the Narcotic Farm, read: "This desperate narcotics addict, caught like his fellows in the revolving door of law enforcement, will probably go back to his habit when he is free."Complete slide show here.
Info on the film here.
Info on the book.
UPDATE: The original article has since issued the following correction:
Correction (posted October 25, 2008): When originally posted, this story suggested that a Congressional investigation into the Narcotic Farm had led to its closure. In fact the main reason Narco was closed was that its centralized form of institutional care was supplanted by a national network of local treatment centers. Its closure coincided with the Congressional investigation into LSD research. Scientific American regrets the error.
Friday, October 24, 2008
Local policy news
Thursday, October 23, 2008
"unexpected findings"
NEW YORK (Reuters Health) - Contrary to expectations, higher intelligence scores at age 10 may be associated with higher levels of alcohol intake and alcohol-related drinking problems during adulthood, study findings suggest.[Thanks Jess]
Moreover, these associations appear "markedly stronger among women than among men," Dr. G. David Batty, from the University of Glasgow in Scotland, and colleagues report in the American Journal of Public Health.
However, "given that these findings ran counter to our expectations," the investigators call for further examination of this relationship.
Batty's team assessed associations between mental ability scores obtained when 8170 boys and girls were 10 years old and their alcohol intake and alcohol problems when they were about 30 years old.
Of the 3895 men and 4148 women who reported drinking alcohol as adults, those with higher average scores on childhood mental ability tests were also more likely to have indications of alcohol problems in adulthood.
The association between higher mental ability in childhood and adulthood problem drinking became stronger among women than among men after allowing for socioeconomic factors such as social class during both childhood and adulthood.
Specifically, for every 15-point increase in childhood mental ability score, the likelihood of drinking problems increased 1.38 times for women, and 1.17 times fro men
These unexpected findings, and the lack of other research in this area, indicate the need for "further examination of the relation between childhood IQ and adult drinking patterns," the investigators conclude.
SOURCE: American Journal of Public Health, October 2008
Monday, October 20, 2008
Local sentencing sense
The defendant, who had been arrested for drunken driving, stood before 15th District Judge Julie Creal.
But unlike a typical sentencing, Creal asked questions of a more personal nature - wondering whether the death of a relative would impact the man's sobriety.
"I'm dealing with it," he said. "It's a tough time for me."
Creal asked how long he'd been sober.
"Sixteen months sober on Tuesday," he replied.
The nearly two dozen people stuffed in Creal's small courtroom for Washtenaw County's Sobriety Court broke into applause.
"Fabulous," Creal said as she clapped.
A judge who applauds? A group of defendants cheering each other's successes?
That's Sobriety Court, created by Creal four years ago to help repeat drunken drivers get treatment. Representatives from the prosecutor's office, city attorney's office, law enforcement and probation department also are present.
People who enter a voluntary, 18-month program and successfully complete it can avoid jail time and save about $1,000 in fines and fees. The program includes random testing at home, attendance at 12-step meetings, making small payments and staying sober.
Since it started, 157 people have entered the program. Of those who are no longer in the system, 60 have completed it successfully - a rate of about 76 percent.
The focus of the program is really about owning up to a problem.
I posted last week about how drug courts and health professional recovery programs are leading the way for the rest of us.
Methadone maintenance as palliative care
As I have said many times before, I have nothing against methadone substitution therapy per se, but I feel strongly about it being used with clients being offered no, or only minimal other, support. I have written:This issue of palliative care gets to the very crux of the issue doesn't it?
'Due to the approach adopted by much of the UK treatment system, this generally leads people from one addiction to another without providing a realistic opportunity to attain recovery.
Whilst methadone (and Subutex) have an important role to play in helping people take the chaos out of a heroin-using lifestyle, they should not be prescribed in isolation or with minimal other support.
The majority of heroin users actually want to get off drugs completely, not be “left” long-term on methadone or other substitute drugs. They must be provided with the choice of, and help in, finding a path to recovery, rather than just being helped to live with addiction. Much of the treatment system shows a shocking paucity of ambition for its clients. If cancer patients were only offered what amounts to a form of palliative care, it would be seen as a scandal.'
From Wikipedia:
The term "palliative care" may be used generally to refer to any care that alleviates symptoms, whether or not there is hope of a cure by other means;It really comes down to whether once believes addiction is a treatable illness doesn't it?
I'd add that it might be possible for a methadone program to have a recovery orientation, rather than a palliative orientation, but it's not what I see.
Once again, I'd welcome a day when addicts are offered recovery oriented treatment of an adequate duration and intensity and have the opportunity to choose for themselves.
Sunday, October 19, 2008
Transformed...beyond hope
The NAOMI study was funded by an $8.1-million research grant from the Canadian Institutes of Health Research.Once again, Emerson comes to mind:
The heroin and hydromorphone participants received three doses a day from health-care professionals in downtown clinics. Most participants - 192 - were from Vancouver. Fifty-nine were from Montreal.
After one year, 90 per cent of the addicts being provided heroin were still in the program and 54 per cent in the methadone program remained - much higher than the retention rates for conventional treatment, Dr. Schechter said.
Researchers said they found a decrease in criminal activity and use of street drugs, and an improvement in health among participants.
Participants must have been addicted to heroin for at least five years and attempted treatment twice in the past.
"This is a group that society has written off as beyond hope," Dr. Schechter said.
This conformity makes them not false in a few particulars, authors of a few lies, but false in all particulars. Their every truth is not quite true. Their two is not the real two, their four not the real four ; so that every word they say chagrins us and we know not where to begin to set them right.Two failed treatments and the best we can hope for is reduced crime, some improvements in health and persistence in showing up to receive free heroin? All for only $32,270 per participant?
Friday, October 17, 2008
Spirituality and recovery
What's especially interesting about this study is that Bill Miller, the lead author, is very friendly to spirituality as an tool for facilitating change. He seems stumped but isn't questioning the study itself.
There is reason for confidence in the findings of this study. Outcome variables were carefully measured by independent interviewers, fidelity of interventions was good, and 82% of all possible follow-up interviews were completed. The studies were powered to detect a medium between-group effect size that would be sufficiently large to be of clinical interest ([Cohen, 1988] and Miller and Manuel (in press) Miller, W. R., and Manuel, J. K. (in press). How large must a treatment effect be before it matters to practitioners? An estimation method and demonstration. Drug and Alcohol Review.Miller and Manuel (in press)). Null findings were replicated across two study designs, and the direction of differences was, in many cases, opposite to prediction. We thus found no evidence for a beneficial effect of this spiritual counseling approach during the acute phase of addiction treatment. Different and more intensive spiritual counseling might increase daily spiritual practices, spiritual experience, and meaning and thereby influence substance use outcomes. Given the magnitude of changes that occur in early recovery, however, we believe that a more promising approach is to focus on spiritual development after a period of stabilization in which other basic needs have been addressed. Within a long-term care perspective, spiritual direction may fit better in later recovery, with a goal of maintaining and broadening the initial gains of sobriety.It would be interesting to see more research on spirituality and recovery. I'm inclined to believe that spirituality can be a useful therapeutic tool. If nothing else, for people when enter treatment with spiritual beliefs, it might be used to increase engagement and participation in treatment. It might also be used as a long term source of support for change. (We do value a holistic approach, right?)
Along the lines of a stage dependent model, as Miller suggests, Project SAFE reported that many of the African American women in the study initiated their recovery in 12 step groups and sustained their recovery in churches.
The study said nothing of the participants' predisposition to spirituality. That seems important to me.
Other questions that might be interesting include:
- What forms of spirituality are helpful or unhelpful? Some clearly emphasize a stronger internal locus of control while others emphasize an external locus of control.
- Can helpful elements of the helpful forms of spirituality be unbundled?
- What are the non-spiritual paths to those helpful elements?
- There is a persistent assumption that all clients will benefit from spirituality. Is this true? Are these some who might benefit, others who are unaffected and some whose treatment outcomes are harmed?
- Along the lines of Miller's thinking, to what degree are these responses stage dependent?
Thursday, October 16, 2008
Early Exposure to Drugs and Alcohol
First, the prior consensus in child psychology and psychiatry has been that adolescents who go on to develop substance dependence are not normal adolescents who are experimenting with substances, but rather are highly likely to be adolescents with a prior history of conduct problems (Armstrong & Costello, 2002). If this is the case, the documented association between early substance exposure and adult outcomes would not be due to exposure per se, but instead would be the result of who is exposed (Wells, Horwood, & Fergusson, 2004). Prior research has not resulted in a consensus regarding the causal status of substance exposure (Agrawal, Neale, Prescott, & Kendler, 2004; Kandel, 2003; Lynskey et al., 2003; Prescott & Kendler, 1999). However, results from this study are consistent with a causal effect of early substance exposure among adolescents with no prior history of conduct problems. That is, early-exposed adolescents with no conduct-problem history, although they did not have an increased risk of failing to complete school, were more likely than their matched non-early-exposed counterparts to develop substance dependence, test positive for herpes, have an early pregnancy, and be convicted of criminal offenses.Strangely, CADCA explains the study by describing some subjects as good kids and the others as bad kids.
Second, findings from this prospective study support a causal link between early substance exposure and a wide range of adult outcomes. Propensity-score-adjusted effects indicate that early substance exposure more than doubles the odds of adult substance dependence, herpes infection, early pregnancy, and criminal convictions.
[hat tip: Jess]
More on Methadone
Wednesday, October 15, 2008
Gone, baby, gone
More sentencing sense
Clearly, the courts do not help everyone. One of the most successful programs is in New York State, where about 1,600 offenders are in adult drug courts. Studies found that while 40 percent dropped out of the program along the way, those who started it, including both dropouts and graduates, had 29 percent fewer new convictions over a three-year period than a control group with similar criminal histories and no contact with drug courts, Mr. Berman said.I'd like Kleiman's proposal if what he describes is a "pre-drug court" that would step addicts up into a full drug court.
In other regions, half or more of those who start the program do not finish. And recidivism rates for participants are reduced by about 10 percent to 20 percent, depending upon the quality of the judges and treatment programs, said John Roman, a researcher at the Urban Institute, based on a recent study.
An earlier review of 57 “rigorous” drug court evaluations around the country, led by Steve Aos of the Washington State Institute for Public Policy, found that recidivism was reduced on average by only 8 percent, but with wide variation.
Yet even that modest reduction in crimes and prison yields cost benefits. The report this year by the Urban Institute found that, for 55,000 people in adult drug courts, the country spends about half a billion dollars a year in supervision and treatment but reaps more than $1 billion in reduced law enforcement, prison and victim costs. A large expansion would yield similar benefits, the report argued.
But some scholars, like Mark A. R. Kleiman, director of the Drug Policy Analysis Program at the University of California, Los Angeles, remain skeptical about the potential and the achievements. He suggests, for example, that success rates of some courts may be inflated because they take in offenders who are not addicted and entered this track only to avoid prison. Dr. Kleiman advocates a slimmed-down system that does not initially require costly treatment, as drug courts do, but simply demands that offenders stop using drugs, with the penalty of short stays in jail when they fail urine tests. Such an approach has shown promise with methamphetamine users in Hawaii, he said, and because it is far cheaper, it can be applied to far more offenders.
How methadone research works
Perform a study offering only two variations of your preferred treatment. (Cheap and crime reducing.) One is high dose or long duration and the other low dose or short duration. Do not offer a recovery oriented option at all, or offer a recovery oriented option of inadequate duration and intensity.
Find that, when offering 2 lousy options, the lousy option with the longer duration or higher intensity reduces symptoms better at follow-up.
Run a headline of, "Methadone Detoxification Remains No Match for Methadone Maintenance, Even with Minimal Counseling." In the comments, declare, "Methadone maintenance is the preferred treatment approach for heroin dependence."
Bonus: "No difference between groups was found for cocaine use or depressive symptoms."
Bonus bonus: "Results for MM with standard counseling (2 hours a month) did not differ from those for MM with minimal counseling (15 minutes a month)."
Question: Do you think this will be used to justify offering even less counseling to methadone recipients?
Five points:
- First, a question. If methadone is a superior treatment option, why don't they use it for opiate addicted health professionals? Health professionals have high rates of opiate addiction and typically receive long term treatment with monitoring that lasts several years. Treatment is stepped up or down as needed. Guess what? They have great treatment outcomes. You might be inclined to chalk it up to a population with lots of recovery capital. To be sure, that plays a role, but surely a real chronic disease management approach plays a role too.
- Second, is it coincidence that this study was done on poor black men? Why aren't studies like this done on young adults from affluent communities?
- Third, methadone used to be one component of some comprehensive bio-psycho-social treatment programs. I understand that there are still some programs that fit this description, but every program in my area is a dosing clinic and little more.
- Fourth, regarding misery, notice that there was no difference in depressive symptoms.
- Fifth, heroin addicts in our long term programs do just as well as everyone else. It's all about hope and expectations. Beware of the subtle bigotry of low expectations.
Tuesday, October 14, 2008
What's possible
By the numbersAn impressive vision. This is a county of 250,000.
Larimer County Issue 1A on the November ballot would levy a 0.25 percent sales tax - or 25 cents on a $100 purchase - to build a facility that would provide treatment for people with mental-health and substance-abuse problems. Below are preliminary figures tied to the proposal:
> $12.5 million: Cost to build the facility
> $5.8 million: Staffing costs for new programs
> $1.3 million: Staffing costs to expand existing programs
> $750,000: Annual medication costs
> $350,000: Annual maintenance and utilities costs
> 41,000 square feet: Size of the building
> 1,200: People who would be served each year
> 72: Staff
Drug Czar = pointless, feckless, hopeless
Maybe it will become a verb, as in, "I've been Drug Czarred!"
Monday, October 13, 2008
Rats, cocaine, memory and volition
Scientists know that addictive drugs can mess with the brain’s circuitry and hijack its reward systems, but a July 31 rat study in the journal Neuron shows that psychological factors may be more instrumental in causing these changes than a drug’s chemical effects are. Cocaine use triggers long-lasting cellular memories in the brain, the study found—but only if the user consumes the drug voluntarily.I posted on this before, but missed this important finding--that the rats involuntarily receiving cocaine did not develop these memory imprints.
A team led by Billy Chen and Antonello Bonci, both at the University of California, San Francisco, trained three groups of rats to press levers that delivered cocaine, food or sugar. The researchers injected cocaine into a fourth group. When they examined the rats’ brain tissue, they found an increase in synaptic strength within the reward center in those rats that had self-administered sugar, food or cocaine. These cellular memories were short-lived in the sugar and food groups, but in rats that had self-administered cocaine they persisted for up to three months after consumption had stopped. Most interestingly, the brains of rats that had consumed cocaine involuntarily did not show such imprints.
The findings illustrate that the pharmacological effects of cocaine alone are not enough to create reward-associated memories, Bonci says. “Instead the motivation for taking the drug seems to be a key component in the process as well.”
The team is working to find ways to remove the long-term cellular memory left by voluntary cocaine use, which eventually could help treat addiction in humans by taking away the desire to actively seek the drug, Chen says.
This is weird. Kind of ironic that volition had to be exercised for the deterioration of volitional control.
Can lab rats become addicted through involuntary cocaine consumption? Or, they just won't develop these imprints? Also worth noting is that behavior extinction had no impact on these cellular memory imprints.
Brain scan skepticism
Good news. This article by a brain scan skeptic says nothing that concerns me.
Sentencing sense
Astonishingly, the article fails to put the import of this in its proper perspective.


Given the state of American drug policy debates, drug courts seem to be the most pragmatic path to ending this insanity. There may come a day when we make more radical changes in drug policy, but, for the time being, drug courts balance concerns about public safety, drug control and the wanton incarceration of people whose primary crime is being an addict.
Thursday, October 09, 2008
The future of treatment spending
Growth in SA spending is forecasted to average 5.0 percent between 2003 and 2014, slightly faster than the rate of 4.8 percent in the 1986-2003 historical period. Over the next decade, SA spending growth is expected to continue to increase at slower rates than MH health spending, mainly because pharmacotherapy, which has driven increases in MH spending, currently plays only a small role in SA treatment. This is expected to result in an SA share that falls from 1.3 to 1.0 percent of all-health spending. Moreover, growth in SA spending increases at a slower pace than growth in the economy, with the SA share of GDP falling slightly between 2003 and 2014.Some of the analysis is already a bit dated, give the recent passage of parity legislation:
Historically, a dominating characteristic of private SA spending has been the lack of funding increases from private health insurance, which declined an average of 1.6 percent annually between 1986 and 2003. We expect private insurance SA spending growth to accelerate somewhat during the projection period--to 1.3 percent annually. However, actual spending in 2014 is anticipated to be below that estimated for 1986, and the private health insurance share of SA spending is expected to continue falling (from 10 percent in 2003 to 7 percent in 2014). Barriers to SA insurance coverage exist that are not present in medical/surgical coverage, including annual and lifetime limits for inpatient hospital stays and outpatient visits, and higher cost sharing through deductibles and coinsurance.Specialty treatment settings are increasingly relied on as a share of spending, but, anecdotally, this makes no sense. Specialty treatment settings are disappearing and McClellan has documented the instability of the treatment system, including high rates of program closure. The definition for SSACs must be pretty inclusive.
Specialty SA centers (SSACs) have emerged as major providers in the delivery of SA treatment, with spending for their services increasing from 19 percent of SA spending in 1986 to a projected 42 percent in 2014. SSACs are multidimensional facilities that deliver services ranging from outpatient care to residential services. Programs can include those targeted to special populations (for example, people with HIV/AIDS or opiate addictions). SA spending on treatment in SSACs is forecasted to increase at a 5.3 percent average annual rate over the projection period, similar to the overall SA annual growth rate between 1993 and 2003.Parity has been passed since this paper was written and it's likely a lot more will change by 2013. It seems likely that some sort of universal coverage be enacted in the next 5 years and we can hope that decent addiction treatment will be covered.
Spending for SA hospital treatment fell from 48 percent of SA spending in 1986 to 24 percent in 2003, where the share is expected to remain in 2014. SSACs likely supplied the outpatient treatment venue for people who previously would have been treated in expensive hospital settings.
Tuesday, October 07, 2008
Insite saves two to 12 lives a year, study says
How many more lives would be saved adding recovery-oriented treatment on demand? How many more lives would be restored? Is Insite lobbying for the addition of these services?
It doesn't have to be either/or. It can be both/and.
Rhythms of despair
Poor prognosis: client fails ==>
Conclusion: these people can't recover ==>
Organize treatment system and research around belief that addicts won't recover ==>
Public and helpers despair at the impotence of the system ==>
They look to research for answers, but research is organized around the assumption that addicts can't recover ==>
They reject the treatment system and the addict:
Street drugs are a lifestyle choice. Being a taxpayer is not; and it is harder to be tolerant of the rotten choices of others when one's hard-earned money is spent subsidizing them long-term.
Some unknown circle of hell
Parity will mean that families with insurance will be able to access treatment but the insurer will implement restrictive protocols for accessing more expensive forms of treatment, like inpatient and residential.
[via dailydose.net]
Monday, October 06, 2008
Win the drug war?
- How can we mitigate the human costs associated with the war on drugs?
- What are we not doing, because we're investing enormous capital and energy in the war on drugs?
- Are there other strategies that might be effective in trying to achieve our goals?
- Are our goals realistic?
Nils Bejerot ... challenged the view ... that addiction was a health problem. ... Bejerot's argument that addiction was a learned behaviour made possible by the availability of drugs, time, money, user role models and a permissive ideology. This behaviour could be "unlearned," he said ...She's right. It's absurd. Ideology is a problem on both sides of the street. It'll be nice when we manage to beyond this false dichotomy.
Saturday, October 04, 2008
Friday, October 03, 2008
Parity passes
This is a good and important step. Health Affairs explains what this means, what will happen next and what still needs to happen:
A thoughtful essay by Audrey Burnam and José Escarce in an earlier volume of Health Affairs contends that the debates around parity in insurance benefits are the latest manifestations of a longer-standing policy issue regarding equity of mental health care relative to general medical care. These authors argue that in an era of managed care, benefit parity is an insufficient mechanism for ensuring equity for those with a mental illness.26 Put another way, full benefit parity is an important "sequential" step toward the broader goal of ensuring that persons with a mental illness or addiction have the same opportunities for seeking and receiving appropriate treatment as those with a physical illness.
Importantly, a sequential approach to promoting treatment equity implies a recognition that full parity resolves some, but far from all, obstacles to access and use of appropriate services among persons with mental and addictive disorders. On the supply side, full parity generally indicates a nominal expansion of benefits. However, parity also has yielded increased management of care, and such management can be differentially applied in ways that produce unequal treatment opportunities (through either initial access or intensity and/or duration of services) for those with psychiatric versus general medical conditions. On the demand side, full parity results in the removal of arbitrary and inequitable limits to treatment. However, removal of these limits under parity may have little effect on the concomitant stigma that keeps many who need mental health and substance abuse services from seeking such care. In short, legislating full parity will promote, but not achieve, treatment equity for those with mental and addictive disorders. Nevertheless, without such action, the goal of equity will continue to remain elusive.
Wednesday, October 01, 2008
Recovery and stigma
30% of respondents said they'd think less of a friend with a drug problem and 18% said they'd think less of a friend in recovery. 66% said that they would be comfortable being friends with someone in recovery, 63% would be comfortable working with someone in recovery and 57% would be comfortable living next door to someone in recovery.
I'm not sure how to feel about this, but I suspect we're supposed to be thrilled. I don't find it very encouraging. Polls about attitudes toward gay people offer more optimistic numbers for gay rights activists and they still face considerable stigma and ballot initiatives in every election cycle.
I understand that this kind of process is important, but I sort of resent people even being asked whether they are comfortable with me. I don't really care if they're comfortable with me. What I do care about is whether they are willing to extend community help and support to the addict who is still suffering. Clearly, we're not there.
I also want to normalize recovery just as much as the next guy, but I'm a little worried that our advocacy of recovery may inadvertently reinforce stigma against active addicts by emphasizing, "We're in recovery! You have nothing to fear from us." As a person in recovery, I don't need anyone's acceptance and I wonder if promoting recovery is really the best way to soften attitudes toward active addicts.
Some of the more troubling findings included that about 40% respondents believe that addicts and alcoholics had only themselves to blame and 42% believe that illicit drug addicts can't recover.
I'm not sure what to make of the prevention attitudes. I suspect SAMHSA finds them encouraging, but I assume that they are more symptomatic of the belief that addiction has a lot to do with a person "losing their way", "getting hooked", or falling in with the wrong crowd."
One more question (to add to the meandering nature of this post). How might current efforts to define "recovery" in a specific, yet inclusive way, affect social attitudes toward addicts?
Okay, another question. Are the motivations to include non-abstinent addicts as "recovering" inclusive compatible with neurobiology and the stigma reduction agenda?
